Suboxone recovery differs fundamentally from traditional abstinence-based approaches by treating addiction as a medical condition rather than a moral choice. You’ll find that while traditional recovery relies heavily on willpower and peer support, Suboxone combines pharmacological intervention with behavioral therapy to address both physical and psychological aspects of addiction. The treatment’s dual-action formula helps manage withdrawal symptoms and reduce cravings, leading to 50% lower overdose rates. Understanding these key differences can shape your path to sustained recovery.
The Science Behind Medication-Assisted Recovery

The science behind medication-assisted recovery (MAR) centers on precisely targeted pharmacological interventions that address opioid dependence at the neurobiological level. Through neurotransmitter modulation, medications like Suboxone work to stabilize your brain chemistry and interrupt the cycle of addiction.
The receptor pharmacology of Suboxone combines buprenorphine’s partial opioid agonist effects with naloxone’s abuse-deterrent properties. While buprenorphine partially activates opioid receptors to reduce cravings and withdrawal symptoms, it doesn’t produce the intense euphoria of full agonists. The naloxone component prevents misuse by triggering withdrawal if the medication is injected. This dual-action mechanism provides a safer, more controlled path to recovery compared to traditional abstinence-based approaches, while effectively managing withdrawal symptoms and reducing relapse risk. Research demonstrates that this approach is more effective than abstinence in reducing opioid use and preventing overdose deaths.
Understanding the Core Treatment Philosophies
While traditional recovery philosophies often emphasize complete abstinence and willpower-based approaches, Suboxone treatment recognizes addiction as a chronic medical condition requiring physiological support through medication. This approach incorporates holistic treatment methods to address both physical and psychological aspects of recovery.
You’ll find that Suboxone’s core philosophy views opioid dependence as a treatable disease rather than a moral choice, supporting long-term recovery through both medication and counseling. Your treatment journey with Suboxone combines medical intervention to manage withdrawal and cravings with behavioral support to address the psychological aspects of addiction. This approach acknowledges that the success of recovery depends on addressing the values and perspectives of each individual patient, rather than solely focusing on brain pathology. Unlike 12-step programs that require participants to surrender to a higher power, Suboxone treatment focuses on evidence-based medical interventions.
Medication vs. Complete Abstinence
Two distinct philosophies dominate modern opioid recovery: medication-assisted treatment using Suboxone (buprenorphine) and complete abstinence approaches. While both aim for recovery, their methods and outcomes differ considerably.
Medication-assisted treatment focuses on stigma reduction through integrated treatment, combining pharmacological stabilization with counseling to reduce cravings and prevent relapse. Treatment plans commonly include behavioral therapies alongside medication to provide comprehensive care. Research suggests that starting patients on doses above 16mg can significantly improve initial treatment engagement and retention. Notably, Suboxone treatment has proven to be the second most effective option for harm reduction and relapse prevention.
The evidence strongly favors medication-assisted approaches. You’ll find that Suboxone treatment cuts overdose mortality by approximately 50% and achieves higher completion rates (65.7%) compared to abstinence-only programs (30.9%). While traditional abstinence programs emphasize complete sobriety, they often report 90%+ relapse rates even with psychosocial support. Suboxone’s ability to manage withdrawal symptoms and reduce cravings provides a more sustainable path to recovery, supported by clinical monitoring and evidence-based protocols.
Physiological Support or Willpower
Understanding core treatment philosophies requires examining how Suboxone and traditional approaches differ fundamentally in their mechanisms for recovery.
While traditional methods emphasize perseverance versus surrender, relying heavily on willpower and emotional healing through support groups, Suboxone takes a medical approach by directly stabilizing brain chemistry. You’ll find that Suboxone’s dual-action formula provides physiological support through buprenorphine’s partial opioid agonism, which manages withdrawal symptoms and cravings without producing euphoria. The naloxone component adds a built-in safeguard against misuse. The medication’s evidence-based design makes it a critical component of comprehensive treatment plans that support long-term recovery. Withdrawal symptoms can begin 12-24 hours after the last dose, making proper medical supervision crucial.
Rather than depending solely on your mental fortitude, Suboxone works at the neurochemical level to maintain recovery. This medical approach acknowledges addiction as a treatable condition requiring sustained receptor occupation, not just behavioral modifications or sheer determination. Treatment can be administered in both inpatient or outpatient settings depending on the severity of addiction and individual patient needs.
Chronic Disease vs. Moral Choice
The fundamental shift in addiction treatment lies in recognizing opioid dependency as a chronic medical condition rather than a moral failing. By reframing addiction through a medical lens, you’ll understand how Suboxone’s approach targets neurobiological mechanisms rather than willpower alone. The treatment’s unique combination of buprenorphine and naloxone helps patients manage withdrawal symptoms while preventing misuse. Treatment often includes outpatient counseling as an essential component of recovery support. Starting with lower doses helps minimize side effects while maintaining the ceiling effect that prevents overdose risk.
| Traditional View | Medical Model |
|---|---|
| Moral weakness | Brain disease |
| Willpower focus | Biological treatment |
| Punishment-based | Evidence-based care |
| Fixed timelines | Individualized treatment plans |
| Abstinence only | Harm reduction approach |
This medical model acknowledges that addiction alters brain chemistry, requiring targeted pharmacological intervention alongside behavioral support. Your recovery journey isn’t about character flaws – it’s about treating a documented health condition with proven medical protocols. This perspective reduces stigma while promoting sustained engagement in treatment, leading to better outcomes through scientifically-validated approaches.
Medical Supervision vs. Peer Support Models
While medical supervision and peer support models represent distinct approaches to opioid recovery, research demonstrates clear advantages for medication-assisted treatment under clinical oversight. When you choose Suboxone treatment, you’ll receive structured medical care beginning with in-office induction, whereas peer support relies primarily on group dynamics and shared responsibilities through community meetings. Recent studies show that medication-assisted treatment reduced overdose risk by 76% in the first three months.
You’ll find that Suboxone treatment integrates both pharmacological support and counseling under physician supervision, offering measurable outcomes and standardized protocols. Abstinence-based models rooted in traditional recovery philosophy from the 1930s have proven less effective than modern medical approaches. The combination of buprenorphine and naloxone helps prevent misuse while effectively managing withdrawal symptoms. Traditional peer support models, though valuable for psychological support, lack medical oversight and standardized outcome measures.
The evidence shows Suboxone users achieve better abstinence rates and experience fewer emergency room visits compared to non-medicated approaches. Through medical supervision, you’ll receive personalized dosing adjustments and monitoring that isn’t available in peer-only support systems.
Accessibility and Treatment Flexibility

Despite significant progress in expanding treatment options, access to Suboxone remains geographically uneven, with 40% of U.S. counties lacking waivered providers as of 2018. This geographic distribution challenge particularly affects rural areas, where there’s a lower density of waivered physicians compared to urban centers.
You’ll find Suboxone treatment offers greater flexibility than traditional programs through office-based care and reduced infrastructure requirements. Recent regulatory changes have removed patient capacity limits and simplified prescribing requirements, making treatment more accessible. The introduction of 100-patient waivers and telehealth options has improved rural access, while community health centers can now integrate addiction treatment into their services.
However, despite these advances, 56% of high-need counties still have inadequate buprenorphine capacity, indicating ongoing challenges in treatment accessibility.
Risk Management and Safety Protocols
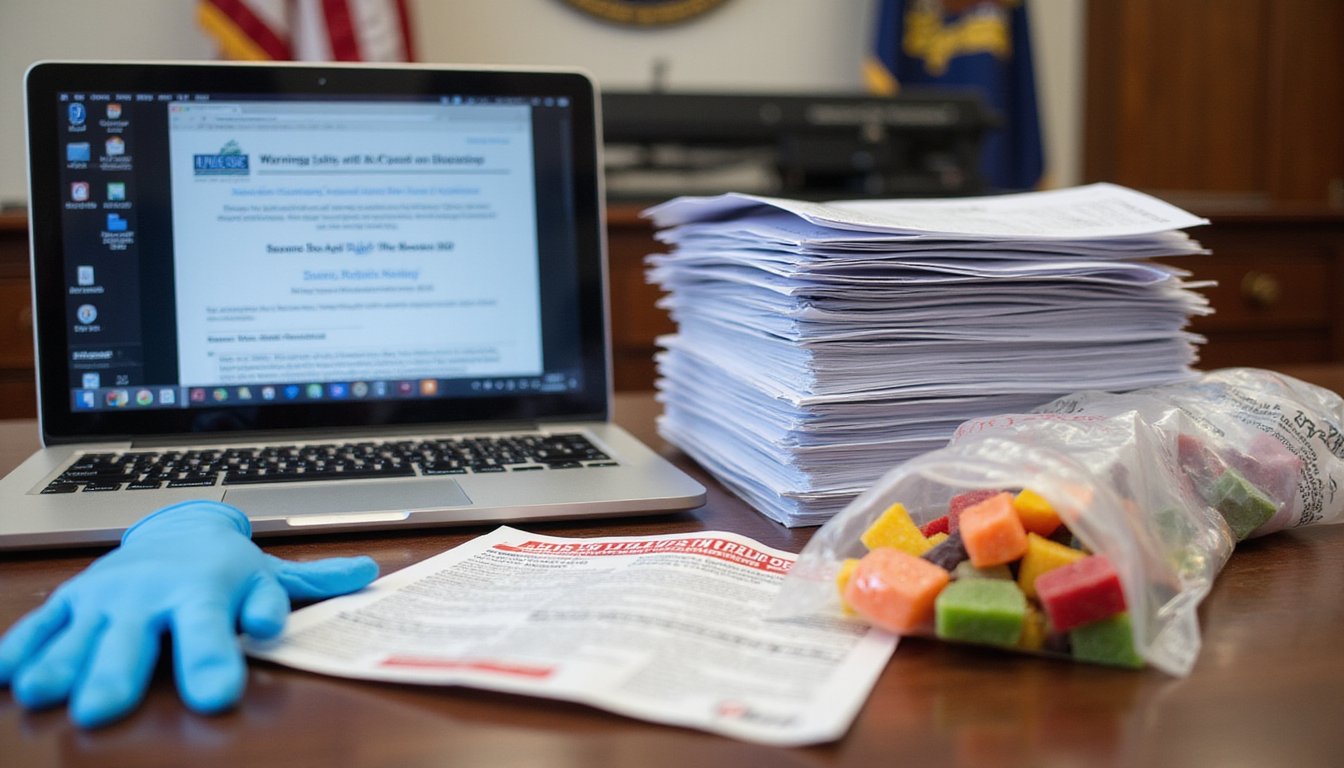
Beyond ensuring treatment availability, implementing robust safety protocols stands at the forefront of Suboxone therapy. You’ll need regular liver function monitoring and must stay vigilant for medication side effects like oral hypoesthesia or nausea. Drug diversion prevention requires secure storage and proper disposal of unused medication.
Your healthcare team will establish clear protocols for managing perioperative pain, including split dosing strategies and alternative pain management approaches like regional anesthesia. They’ll also monitor potential interactions with other opioids, as Suboxone can precipitate withdrawal in patients dependent on full agonists.
You’ll receive education about early warning signs of liver dysfunction and proper sublingual administration techniques. If you’re planning surgery, your provider will develop a specialized plan that may include temporary medication adjustments.
Managing Physical Dependencies and Withdrawal

The shift from traditional opioids to Suboxone requires careful management of physical dependencies and withdrawal symptoms. You’ll need to meet specific clinical criteria, including a COWS score of 6 or higher and observable withdrawal signs, before starting treatment. This evidence-based approach helps prevent precipitated withdrawal and supports ideal patient outcomes.
Medication administration protocols for Suboxone differ vastly from traditional recovery methods. You’ll receive your doses under direct pharmacist supervision, supporting patient centered care goals while minimizing diversion risks. The partial agonist properties of buprenorphine provide controlled withdrawal management with a lower risk of respiratory depression compared to full opioids.
Unlike traditional recovery’s complete abstinence approach, Suboxone offers a structured, pharmacologically-supported alteration that addresses both physical dependencies and withdrawal challenges systematically.
Long-Term Recovery Strategies
Long-term Suboxone treatment challenges traditional abstinence-only models by recognizing that some patients benefit from extended maintenance rather than complete cessation.
You’ll work with your healthcare provider to determine an individualized treatment duration based on your stability, withdrawal severity, and progress in addressing underlying psychological factors.
Your treatment plan may extend for months or years, allowing for gradual tapering while you develop robust coping mechanisms through concurrent behavioral therapy.
Maintenance Vs Complete Abstinence
When considering recovery from opioid dependence, evidence strongly favors maintenance therapy with Suboxone over complete abstinence approaches. Research shows that maintenance treatment prevents relapse in about two-thirds of patients, while abrupt discontinuation leads to a 62% relapse rate within six months.
Medication adherence in Suboxone programs yields markedly better outcomes, with 76.7% achieving opioid abstinence compared to 63.5% in traditional treatment. To maintain lifestyle balance, structured monitoring and incentivized take-home medication privileges can enhance your compliance. While traditional abstinence-based programs emphasize peer support and 12-step models, they often struggle to address the physiological aspects of dependence.
Your success in either approach depends on treatment duration, social support networks, and personal factors like age of first use and impulsivity levels.
Treatment Duration Expectations
Treatment duration for Suboxone varies considerably among individuals, with research showing episodes lasting anywhere from several months to multiple years. Data driven outcomes indicate that longer retention correlates with better recovery success, as 50.8% of patients report 12-month abstinence with extended treatment.
Treatment continuation challenges often emerge during the first year, with only 24-48% of episodes meeting standard retention criteria. While some patients achieve stability within months, others require years of maintenance for ideal results. Your treatment timeline should be based on personal factors including relapse risk, mental health status, and life circumstances rather than predetermined endpoints. The evidence suggests that rushing to discontinue treatment can increase relapse risks, making it essential to work with your healthcare provider to determine appropriate duration.
Breaking Down Social Perceptions
Social stigma continues to be one of the most significant barriers facing individuals using Suboxone for opioid use disorder (OUD). You’ll likely encounter misconceptions about your self perception and public image during treatment, as research shows significant societal resistance to medication-assisted recovery.
| Perception | Traditional View | Medical Reality |
|---|---|---|
| Treatment Type | “Substituting drugs” | Evidence-based medicine |
| Recovery Status | “Not truly clean” | Managing chronic condition |
| Causation | Personal weakness | Medical disorder |
| Support Needs | Willpower alone | Extensive care |
| Success Metrics | Complete abstinence | Harm reduction & stability |
Despite medical evidence supporting Suboxone’s effectiveness, only 49% of Americans believe in successful long-term OUD treatment. You’re facing a landscape where traditional recovery philosophies often conflict with modern medical approaches, potentially impacting your treatment journey and social support options.
Treatment Success Metrics and Outcomes
Understanding success metrics in Suboxone treatment requires examining multiple evidence-based indicators beyond traditional abstinence measures. You’ll find that retention rates show 75% of patients remain in treatment after 24 weeks, with participants 1.82 times more likely to stay engaged compared to non-MAT approaches.
Engagement metrics demonstrate a 14.2% reduction in opioid-positive tests, while higher buprenorphine doses correlate with improved outcomes. For relapse prevention, Suboxone proves 1.8 times more effective than non-medicated paths, particularly in reducing overdose risks and illicit opioid use.
Long-term success indicators include successful shifts to primary care and sustained medication adherence. These outcomes profoundly outperform traditional recovery methods, emphasizing Suboxone’s effectiveness in managing opioid use disorder as a chronic condition rather than pursuing abstinence alone.
Frequently Asked Questions
Can Suboxone Patients Safely Undergo Surgery or Receive Pain Medication?
Yes, you can safely undergo surgery while on Suboxone, but it requires careful planning with your medical team. Your perioperative pain management will need special consideration due to Suboxone’s strong binding to opioid receptors.
You’ll need to work with your doctors to either pause Suboxone before surgery or use alternative pain control methods. Postoperative opioid use is possible with proper coordination between your surgeon, anesthesiologist, and addiction specialist to guarantee safe, effective pain management.
How Does Pregnancy Affect Suboxone Treatment Options and Safety?
You can continue Suboxone treatment during pregnancy, as abruptly stopping could risk withdrawal and harm fetal development. While research shows buprenorphine is generally safe during pregnancy, you’ll need close monitoring and possible dose adjustments as your pregnancy progresses.
Discuss breastfeeding considerations with your healthcare provider, as limited data exists on Suboxone’s effects during lactation. You’ll work with your doctor to balance treatment benefits against potential risks throughout your pregnancy.
What Role Do Family Members Play in Suboxone Versus Traditional Recovery?
In Suboxone treatment, your family plays a more structured clinical role, actively participating in medication management and therapeutic interventions. You’ll find that family involvement directly impacts treatment success, with studies showing a threefold increase in completion rates.
Unlike traditional recovery’s peer support group focus, where family members mainly provide emotional backing, Suboxone programs integrate your family into treatment planning, medication compliance, and ongoing therapy sessions through both in-person and digital platforms.
Are There Specific Dietary Restrictions While Taking Suboxone?
You don’t need to follow specific dietary restrictions while taking Suboxone. Clinical studies haven’t shown any mandatory food limitations or interactions.
It’s best to wait 30-60 minutes after taking Suboxone before eating to guarantee proper absorption. While some providers may recommend nutritional supplements to support overall health, there’s no evidence-based dietary guidance unique to Suboxone treatment.
Focus on maintaining balanced nutrition and staying well-hydrated throughout your recovery process.
Can Suboxone Treatment Be Covered by Insurance or Medicare?
Yes, you’ll find that Suboxone treatment is widely covered under various healthcare coverage options. Most private insurance plans, Medicare Part D, and Medicaid include Suboxone in their medication management protocols.
While prior authorization may be required, you can typically access both brand-name Suboxone and generic alternatives. Your out-of-pocket costs will vary depending on your plan, but patient assistance programs and generic options can help reduce expenses considerably.