Smoking addiction stems from nicotine’s precise targeting of your brain’s acetylcholine receptors, triggering dopamine release in the nucleus accumbens – your reward center. When you smoke, nicotine rapidly hijacks these neural pathways, creating powerful dependence through neuroadaptive changes that alter receptor sensitivity and strengthen drug-reward connections. Your genetic makeup influences addiction susceptibility by 40-75%, while environmental triggers intensify cravings through stress-activated neural circuits. Understanding these neurological mechanisms reveals the intricate pathways to breaking nicotine’s grip.
The Brain’s Reward System and Nicotine
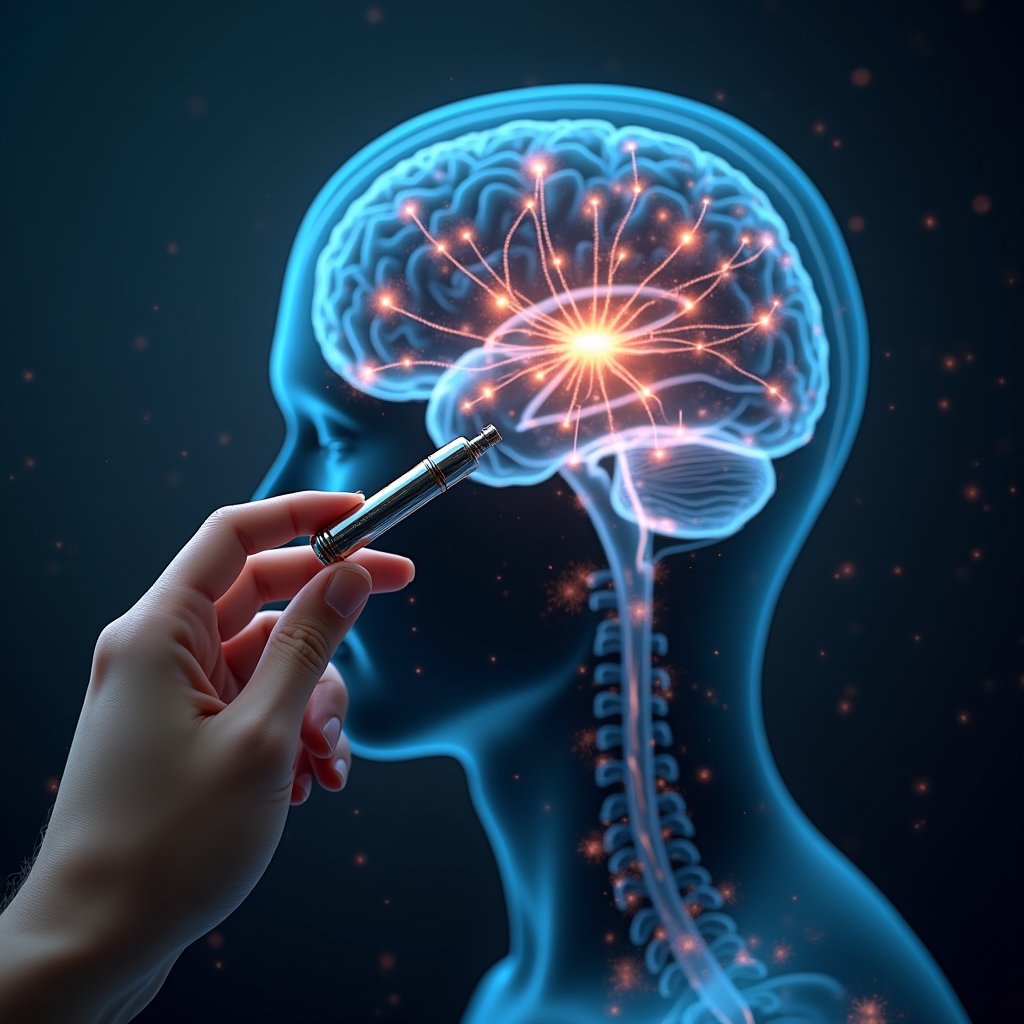
When nicotine enters the brain, it primarily targets nicotinic acetylcholine receptors (nAChRs), triggering a cascade of neurological events that establish and maintain addiction.
These receptors, particularly the α4 and β2 subunits, are densely expressed in your brain’s reward-relevant neurons within the ventral tegmental area (VTA).
Your neural reward system responds as nicotine activates dopaminergic neurons through nAChR stimulation, leading to dopamine release in the nucleus accumbens.
This process forms the core of addiction mechanisms, where both GABAergic and glutamatergic systems interact to modulate reward processing.
Recent research confirms that VTA glutamate neurons directly respond to nicotine, adding another layer to our understanding of addiction pathways.
You’ll experience heightened alertness and arousal through locus coeruleus activation, while prefrontal cortex modulation affects your decision-making abilities.
Multiple nAChR subtypes, including those with β3, α6, or α5 subunits, influence distinct aspects of nicotine’s stimulatory effects on your brain.
Nearly half of those who experiment with cigarettes develop chronic nicotine dependence, highlighting the highly addictive nature of tobacco products.
Dopamine: The Key Player in Smoking Addiction

Through intricate dopaminergic mechanisms, nicotine orchestrates a complex neurochemical cascade that forms the cornerstone of smoking addiction. When you smoke, nicotine binds to specific receptors, triggering dopamine release via multiple pathways, particularly in your brain’s reward centers. Studies show that nucleus accumbens activation plays a central role in reinforcing continued tobacco use.
Your genetic variations in MAO A/B and nAChR subunits influence how intensely you’ll respond to nicotine’s effects. The interplay between neurotransmitter interactions becomes evident as nicotine improves glutamate release while suppressing GABA, creating a perfect storm for dopamine surge. Recent studies documented in pharmacogenomics databases have enhanced our understanding of these genetic variations.
Over time, your receptor sensitivity diminishes, requiring more nicotine to achieve the same effect. This process involves complex cross-talk between dopamine pathways and other neurotransmitter systems, including serotonin and norepinephrine. The resulting neuroplastic changes in your brain’s dopamine circuits perpetuate the cycle of addiction and withdrawal.
How Nicotine Hijacks Neural Pathways

Inside your brain’s reward circuitry, nicotine initiates a sophisticated cascade of neural adaptations by binding to specific nicotinic acetylcholine receptors (nAChRs) in the ventral tegmental area (VTA).
When nicotine receptor activation occurs, it triggers ion channels that depolarize dopamine neurons while simultaneously modulating glutamate and GABA release. The quick depletion of nicotine from the body creates intense recurring cravings that drive continued use.
This neural circuit rewiring creates lasting changes in your brain’s architecture. The process involves multiple mechanisms: stimulation of glutamatergic terminals improves dopamine release in the nucleus accumbens, while GABAergic interneurons become inhibited, further elevating dopamine levels.
Your brain’s mesolimbic pathway undergoes significant alterations, shifting from natural reward processing to drug-driven reinforcement. Furthermore, chronic exposure leads to nAChR upregulation, strengthening pathological connections between drug use and reward signals, while compromising your prefrontal cortex’s inhibitory control mechanisms.
The Science Behind Smoking Cravings
Your brain’s dopamine reward pathways become markedly altered through nicotine exposure, as smoking triggers rapid neurotransmitter releases that reinforce addictive patterns through mesolimbic circuits.
When you stop smoking, your upregulated nicotinic acetylcholine receptors undergo a challenging reset period, intensifying withdrawal symptoms and craving responses. Research shows that smokers experiencing withdrawal tend to seek high-calorie foods as a coping mechanism.
Stress-induced cortisol release further complicates this process by activating neural circuits associated with nicotine seeking, making you particularly vulnerable to cravings during high-pressure situations.
Dopamine’s Reward System Impact
The intricate relationship between nicotine and dopamine lies at the heart of smoking addiction‘s powerful grip. When you smoke, nicotine directly activates dopamine neurons in your ventral tegmental area, triggering immediate dopamine fluctuations throughout your brain’s reward centers. This activation produces dopamine surges that are ten times stronger than natural rewards.
These surges create intense pleasure sensations that your brain quickly learns to associate with smoking. Through repeated exposure, your reward reinforcement pathways undergo significant changes. Your brain’s nicotinic receptors increase in density, requiring more nicotine to achieve the same dopaminergic effect.
Meanwhile, nicotine’s ability to inhibit MAO enzymes prolongs dopamine availability, further strengthening addiction patterns. Your amygdala and hippocampus become hypersensitive to smoking cues, while dopamine disruption in your prefrontal cortex impairs your ability to resist cravings, creating a self-perpetuating cycle of dependence. Statistics show that while 70% of smokers want to quit, breaking free from this neurological cycle proves challenging for many.
Brain Receptor Reset Cycles
When nicotine repeatedly floods your brain’s receptors, it triggers a complex cascade of neuroadaptive changes that establish persistent craving cycles. Through chronic exposure, your brain undergoes receptor upregulation, creating more nicotinic receptors while simultaneously reducing their sensitivity. Smokers can develop billions more receptors compared to non-smokers, intensifying addiction.
This neuroplasticity adaptation disrupts normal acetylcholine signaling, forcing your brain to compensate. The ventral tegmental area shows increased dopamine neuron firing and bursting patterns during nicotine exposure. Physical exercise can help restore balanced dopamine signaling during withdrawal.
When you quit smoking, this delicate balance collapses. Your heightened receptor dynamics, combined with neurotransmitter imbalance, intensify withdrawal sensitivity.
The excess receptors you’ve developed become hyperresponsive, amplifying craving mechanisms. Your brain’s dependence cycles have been fundamentally altered through receptor hypersensitivity, making you more vulnerable to relapse.
This biological rewiring explains why breaking free from nicotine addiction requires more than just willpower – it demands time for your brain’s receptor systems to reset.
Stress-Triggered Nicotine Urges
While experiencing acute stress, interconnected neurobiological mechanisms trigger intense nicotine cravings through multiple pathways. Your brain’s stress responses activate CRF-CRF1 systems, disrupting emotional regulation and boosting addiction cycles. You’ll experience cognitive impairments as stress diminishes your dlPFC’s ability to maintain impulse control. Studies show that up to 75% of smokers relapse within six months of quitting due to these stress-triggered mechanisms. The negative effects are devastating, with tobacco-related deaths claiming 1,200 American lives every day. Smokers develop increased tolerance levels over time, making it progressively harder to achieve stress relief through nicotine use.
| Stress Factor | Neurological Impact | Craving Effect |
|---|---|---|
| CRF Release | CRF1 Receptor Activation | Elevated Nicotine Seeking |
| Cortisol Surge | Reduced dlPFC Function | Weakened Resistance |
| Norepinephrine | Disrupted Glutamate | Impaired Decision-Making |
| Emotional Distress | Increased Dopamine | Intensified Urges |
| Withdrawal | CRF System Activation | Compulsive Use |
Your neurological pathways respond to behavioral triggers through hormonal interactions, as stress-induced withdrawal effects create a self-perpetuating cycle of craving mechanisms and nicotine dependency.
Genetic Risk Factors in Tobacco Dependence
Scientists now understand that genetic risk factors play a substantial role in tobacco dependence through complex polygenic inheritance patterns. Your genetic heritability for nicotine addiction ranges from 40-75% based on standardized FTND scores, with specific component traits like time to initial cigarette showing even stronger genetic influences of up to 68%.
Key gene variants, particularly in the CHRNA5-CHRNA3-CHRNB4 cluster, directly impact your susceptibility to heavy smoking and heightened dependency. Each risk allele you carry correlates with smoking approximately 1.2 more cigarettes daily. Recent research has shown that higher polygenic scores for conditions like schizophrenia, depression, and neuroticism indicate increased nicotine dependence risk.
Your genetic profile also influences associated traits like risk-taking behavior, anxiety levels, and educational attainment – all of which contribute to dependency risk through shared biological pathways. This complex interplay of multiple genes shapes your individual vulnerability to tobacco addiction.
Neuroadaptation and Tolerance Development
When you consume nicotine, your brain’s nicotinic acetylcholine receptors (nAChRs) undergo rapid desensitization, triggering compensatory upregulation to maintain neural function.
Chronic exposure leads to robust up-regulation of α4β2 receptors in key reward circuits of the brain.
Your dopaminergic system adapts through increased nucleus accumbens release capacity and altered clearance mechanisms, while GABAergic circuits show reduced inhibitory neurotransmission.
These neuroadaptive changes progressively raise your tolerance threshold, requiring escalating nicotine doses to achieve the same physiological and psychological effects that previously occurred at lower doses. This process diminishes responses to natural rewards while activating what scientists call an antireward system tied to stress responses.
Brain Changes During Exposure
Through prolonged nicotine exposure, your brain undergoes significant neuroadaptive changes across multiple circuits and regions. Your functional brain connectivity shifts dramatically, with reduced activity in cognitive control areas and heightened sensitivity in reward pathways. With continuous use, nicotinic receptors increase, leading to tolerance development and altered brain function.
| Brain Region | Nicotine Impact |
|---|---|
| Prefrontal Cortex | Decreased activity, impaired decision-making |
| Nucleus Accumbens | Improved dopamine release, reward processing |
| Anterior Cingulate | Reduced connectivity, altered craving control |
| Temporal Lobes | Decreased grey matter volume |
| Striatum | Heightened withdrawal reactivity |
These structural changes manifest through reduced grey matter in key cognitive areas, while withdrawal effects trigger increased connectivity in reward circuits. Neurochemical adaptations include receptor downregulation and altered neurotransmitter release. Functional imaging reveals how smoking suppresses neural responses to craving-related stimuli while simultaneously improving pathways linked to cognitive performance, demonstrating your brain’s complex compensatory mechanisms.
Escalating Dosage Requirements
The brain’s structural adaptations to nicotine set the stage for a complex pattern of escalating dosage requirements. Your central nervous system undergoes significant neuroadaptations as you continue smoking, leading to escalating tolerance that demands higher nicotine levels to achieve the same effects.
- Your neuronal nicotinic acetylcholine receptors (nAChRs) become rapidly desensitized, requiring progressively larger doses to overcome this reduced responsiveness. Individuals show great interindividual variability in how quickly they develop tolerance to nicotine’s effects. The repeated exposure to nicotine creates pleasure responses in the brain that reinforce continued use.
- Chronic exposure triggers compensatory receptor adjustments, fundamentally altering your physiological threshold for nicotine’s effects.
- Your brain’s adaptive neuroplasticity diminishes aversion signals while simultaneously upregulating neurotransmitter systems like GABA and serotonin to counteract nicotine’s disruption.
These dosage adaptations create a self-perpetuating cycle where you’ll need increasingly higher nicotine concentrations to maintain the desired neurochemical effects.
The Morning Cigarette Phenomenon
Smoking within minutes of waking represents one of the strongest behavioral indicators of severe nicotine dependence, with time to initial cigarette (TTIC) serving as a critical metric in addiction assessment. Your morning cravings reflect an automated, deeply ingrained neural response, where habitual smoking patterns have rewired reward circuitry to prioritize nicotine intake immediately upon consciousness.
| Time to Initial Cigarette | Risk Level |
|---|---|
| Within 5 minutes | Severe Risk |
| 6-30 minutes | High Risk |
| 31-60 minutes | Moderate Risk |
| Over 60 minutes | Lower Risk |
| Variable timing | Inconsistent Risk |
Research demonstrates that you’re three times more likely to develop lung cancer if you smoke within five minutes of waking, regardless of your daily consumption. This phenomenon stems from heightened carcinogen absorption due to more intense smoking behaviors during these early morning sessions.
Brain Chemistry Changes During Withdrawal
When nicotine withdrawal begins, your brain undergoes dramatic neurochemical shifts that disrupt multiple neural circuits simultaneously. Your dopamine signaling becomes severely dysregulated, with decreased activity in reward centers but paradoxical increases in your prefrontal cortex. These neurochemical imbalances trigger intense cravings while amplifying anxiety and stress responses.
- Your cognitive deficits emerge within hours, affecting working memory, sustained attention, and response inhibition.
- Your amygdala becomes hyperactive, intensifying negative emotions while your prefrontal cortex struggles to regulate them.
- Your brain’s reward pathways prioritize nicotine-seeking over natural rewards, while stress systems release excess cortisol.
The severity of these changes varies based on your genetic predispositions and receptor density, with symptoms typically peaking 24-72 hours after cessation. Your brain gradually rebalances as receptor normalization occurs post-cessation.
Environmental Triggers and Neural Response
Beyond internal neurochemical shifts, environmental factors powerfully shape your brain’s response to nicotine addiction through complex interactions with neural circuits. Your neural pathways become sensitized to environmental cues through repeated exposure, particularly in areas with high tobacco retail density. These triggers activate reward circuitry and intensify craving responses.
| Environmental Factor | Neural Impact |
|---|---|
| Retail Visibility | Activates reward anticipation |
| Neighborhood stress | Raises cortisol response |
| Social smoking cues | Triggers mirror neurons |
| SES deprivation | Alters stress reactivity |
| Physical access | Strengthens habit circuits |
Your brain’s susceptibility to these triggers varies based on genetic predisposition and epigenetic modifications. Living in areas with heightened neighborhood stress can increase your neural stress response, making you more vulnerable to smoking as a coping mechanism. This creates a feedback loop between environmental exposures and neural adaptations.
Breaking the Cycle: Neurological Perspectives
Understanding how to break nicotine’s neurological grip requires examining the complex interplay between receptor desensitization and dopaminergic reinforcement pathways. Your brain’s neurological feedback mechanisms have adapted to nicotine, creating persistent addiction cycles that resist change.
Breaking free from nicotine means understanding how your brain’s adaptations and reward systems work together to maintain addiction’s powerful hold.
When you attempt to quit, you’re battling both receptor reorganization and altered reward circuitry.
- Your nAChR receptors need time to resensitize, requiring a complete break from nicotine to restore normal acetylcholine function.
- Your dopamine system must rebalance, which includes regenerating D2 receptor density and normalizing reward thresholds.
- Your prefrontal cortex requires strengthening to rebuild impulse control and override automated smoking responses.
Breaking these cycles involves targeted interventions that address multiple neurotransmitter systems simultaneously, including GABA, serotonin, and norepinephrine pathways, while allowing neural circuits to reestablish pre-addiction patterns.
Frequently Asked Questions
How Does Nicotine Interact With Other Recreational Drugs in the Brain?
When you consume nicotine alongside recreational drugs, you’re activating complex neurological interactions.
Through HDAC inhibition, nicotine boosts cocaine‘s effects on your brain’s reward circuits. You’ll experience amplified dopamine release in the nucleus accumbens when combining substances, as nicotine primes your neural pathways.
The drug interactions create synergistic effects through shared dopaminergic systems, while glutamate signaling becomes elevated, potentially intensifying the rewarding properties of both substances.
Can Brain Chemistry Permanently Return to Normal After Quitting Smoking?
Yes, your brain chemistry can largely return to normal after quitting smoking, though the timeline varies.
You’ll experience withdrawal symptoms as nicotinic receptors downregulate and dopamine systems rebalance.
Brain recovery typically progresses through distinct phases: acute withdrawal (days), neuroadaptation (weeks), and long-term restoration (months).
While most neural circuits normalize within 1-2 years, some subtle receptor changes may persist, particularly if you’ve smoked long-term.
Why Do Some People Become Addicted Faster Than Others?
Your susceptibility to rapid nicotine addiction depends on both genetic factors and environmental influences.
If you carry specific variants of the CHRNA5-CHRNA3-CHRNB4 gene cluster, you’ll likely develop dependence more quickly.
Your CYP2A6 gene affects how fast you metabolize nicotine, while variations in your dopamine pathway genes can make you more sensitive to nicotine’s rewarding effects.
Environmental stressors and early exposure through peer influence can accelerate this addiction process.
Does Secondhand Smoke Exposure Affect Brain Chemistry Similarly to Active Smoking?
Yes, secondhand smoke greatly alters your brain chemistry in ways that parallel active smoking.
When you’re exposed, nicotine readily crosses your blood-brain barrier, binding to the same dopamine receptors and triggering similar neurochemical cascades.
PET scan studies show identical receptor occupancy patterns, and you’ll experience immediate measurable changes in neurotransmitter release.
Your brain’s response to secondhand exposure mirrors active smoking’s effects, just at lower concentrations.
How Does Age of First Cigarette Impact the Strength of Addiction?
When you smoke your initial cigarette before the threshold of 18, you’re 2.15 times more likely to develop strong nicotine addiction compared to starting at 21+.
Your developing brain‘s heightened plasticity makes you particularly vulnerable, as early exposure rewires neural pathways for long-term dependency.
You’ll face more severe addiction strength because your teenage prefrontal cortex is still maturing, making you more susceptible to nicotine’s neurochemical effects and creating persistent reward circuitry alterations.